Your Body´s Security Team Fights Cancer – Differences between CAR-T, checkpoint inhibitors, and other immunotherapies
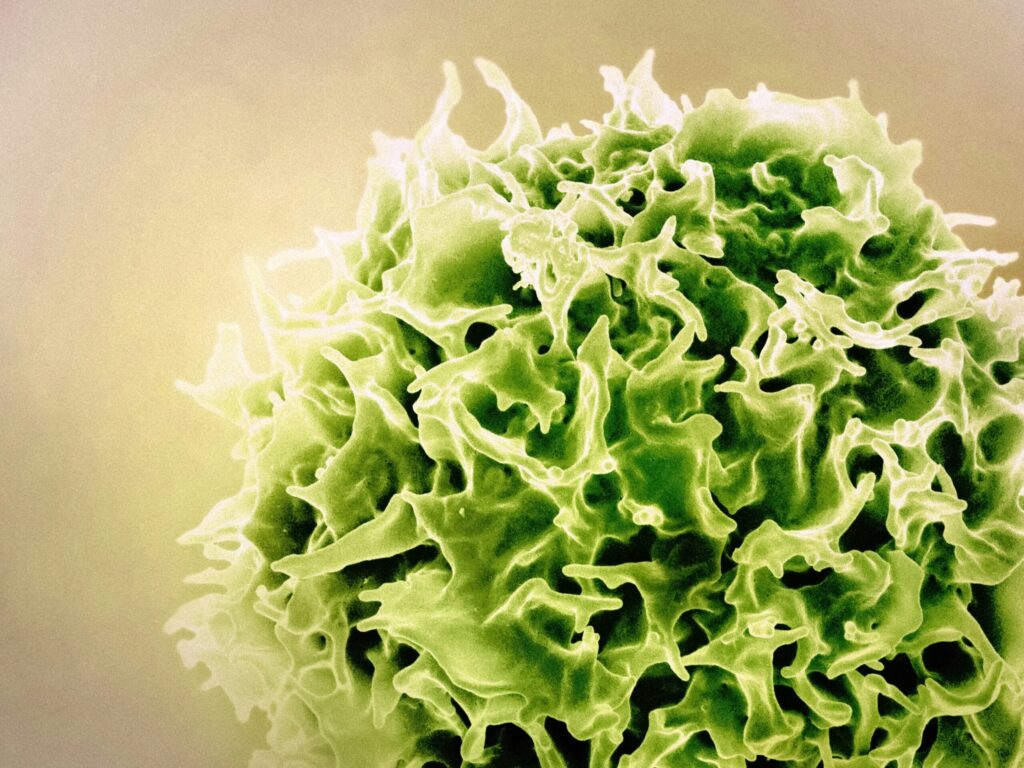
Cancer is like a master criminal, finding ways to outsmart the body’s natural defenses. Normally, the immune system acts like a highly trained security force, patrolling for threats and eliminating dangerous cells. But cancer is different. It disguises itself as normal, hijacks security checkpoints, and builds safe zones where it can grow unchecked.
This is where immunotherapy steps in. Unlike chemotherapy, which attacks both healthy and cancerous cells, immunotherapy arms the immune system with smarter tools. Different immunotherapies work in different ways. To make them easier to understand, think of them as different security strategies used to catch criminals.
CAR-T Therapy: Training an Elite Special Forces Unit
Some criminals are so dangerous that regular security officers can’t handle them. Instead, a city calls in a specialized SWAT team trained for the mission. That’s how CAR-T therapy works.
Doctors remove T cells—the body’s natural security officers—from a patient’s blood. In a lab, they reprogram these cells to recognize and attack a specific cancer marker. Once trained, the enhanced T cells return to the body, ready to hunt down cancer cells.
This method is highly effective against certain blood cancers like leukemia and lymphoma. But, just like a SWAT team is only useful for specific high-risk missions, CAR-T therapy works best when doctors can identify a clear target on cancer cells.
Checkpoint Inhibitors: Unlocking Handcuffed Security Guards
A well-run security force doesn’t attack randomly. Officers follow strict rules to avoid harming innocent civilians. The immune system has similar built-in brakes, called checkpoints, to prevent it from attacking healthy cells. But cancer exploits these checkpoints, tricking immune cells into standing down when they should be fighting back.
Checkpoint inhibitors remove these restraints, allowing the immune system to act. The most well-known checkpoints involve PD-1, PD-L1, and CTLA-4. Here’s how they work:
- PD-1 (Programmed Death-1): The Facial Recognition Scanner
- PD-1 is a checkpoint found on immune cells (T cells). Think of it as a facial recognition scanner that ensures security officers only target criminals.
- PD-L1 (Programmed Death-Ligand 1): The Fake ID Scam
- Some cancer cells produce PD-L1, which binds to PD-1 and tricks immune cells into thinking they are harmless. It’s like a criminal using a fake ID to get past security.
- CTLA-4 (Cytotoxic T-Lymphocyte-Associated Protein 4): The Security Clearance Problem
- CTLA-4 works earlier in the immune response, limiting how many security officers (immune cells) can be on duty at once. Cancer keeps the immune system understaffed, preventing a full-scale attack.
Checkpoint inhibitors, like pembrolizumab (Keytruda) and nivolumab (Opdivo), block these tricks. Once the restraints are lifted, the immune system can recognize and destroy cancer cells.
Cytokines: The Emergency Alert System
Sometimes, security officers know there’s a threat but lack coordination. They need a loud, clear signal to act. This is where cytokines come in—small proteins that work like an emergency alert system, calling reinforcements when needed.
- Interleukins (IL-2): Mobilizing the Troops
- IL-2 acts like a city-wide radio broadcast, alerting all security forces to respond immediately. It helps activate T cells to fight cancer.
- Interferons (IFN-α): The High-Tech Surveillance System
- IFN-α functions as an advanced surveillance network, detecting suspicious activity and alerting immune cells to respond faster. It makes the immune system more effective at fighting cancer and infections.
Doctors sometimes inject high doses of cytokines to boost the body’s defense system, making it stronger and more responsive against cancer.
Other Immunotherapies: Expanding the Security Strategy
Beyond CAR-T therapy, checkpoint inhibitors, and cytokines, other immunotherapy strategies add extra layers of defense.
Cancer vaccines act like neighborhood watch programs, training the immune system to recognize cancer before it becomes a bigger problem. Monoclonal antibodies serve as undercover agents, latching onto cancer cells to mark them for destruction or block their growth signals. Meanwhile, oncolytic viruses operate like controlled demolitions, infecting and bursting cancer cells from the inside out while leaving healthy cells untouched.
A Smarter, Stronger Defense Against Cancer
Cancer is not a simple enemy. It constantly changes tactics to evade detection. That’s why immunotherapy doesn’t rely on just one strategy—it builds a multi-layered defense. From elite special forces (CAR-T), freeing security officers (checkpoint inhibitors), sending emergency alerts (cytokines), to neighborhood watch programs (vaccines), these treatments empower the immune system to fight smarter.
For patients considering immunotherapy, understanding how these treatments work can be reassuring and empowering. While every treatment journey is unique, one thing is clear—modern medicine is giving the body’s security team better tools to win the fight against cancer. If you or a loved one is exploring immunotherapy, speak with your doctor about which approach might be best for you.