Is Your Brain’s Fireplace Burning Too Hot?
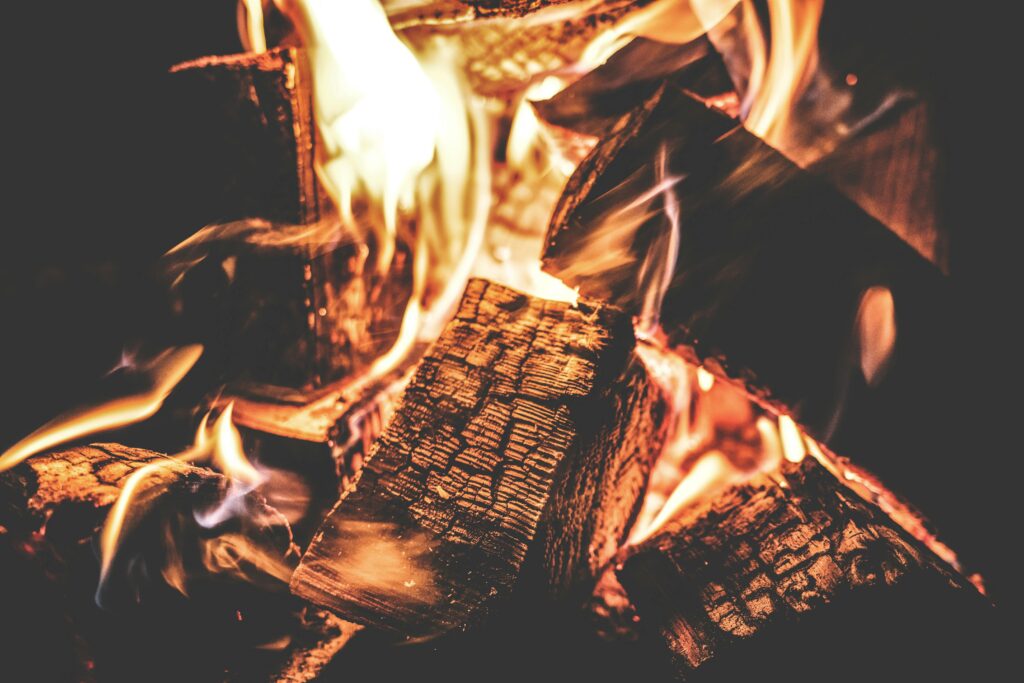
Imagine your brain as a fireplace—a source of warmth and energy that must burn consistently to keep everything running smoothly. But not all fuels burn the same way. Some burn clean and steady, while others choke the chimney with smoke or even send sparks flying, threatening to engulf the whole house in flames.
For years, debates have raged over what’s driving chronic inflammation and diseases like Alzheimer’s. Is it fat, slowly clogging the system? Is it glucose, burning too hot and fast? Or is there an invisible accelerant—like fructose, quietly turning a controlled fire into an inferno?
This article takes a deep dive into the latest research, challenging conventional wisdom on fat and carbohydrate metabolism, and explores whether extreme diets like keto are really superior to more balanced approaches.
Are Fats Clogging the Chimney or Keeping the Fire Steady?
For decades, dietary fat was blamed for heart disease, obesity, and inflammation. The logic seemed simple: Eat fat, and it gets stored. Eat too much, and it clogs your blood vessels and inflames your body, including the brain.
Some research still supports this concern:
- Saturated fats have been linked to higher levels of neuroinflammation and cognitive decline, particularly in people carrying the ApoE4 gene variant, which increases the risk for Alzheimer’s
- Trans fats (found in processed foods) are unquestionably harmful, raising inflammation markers and damaging blood vessels
But newer research challenges this idea. Fats don’t act alone—their effects depend on the context of the diet:
- Omega-3 fatty acids (from fish and nuts) actually reduce neuroinflammation
- Ketogenic diets, which replace carbs with fats, have shown promise in protecting brain function by improving mitochondrial efficiency
So, are fats the problem? It depends on what kind.
Processed fats clog the chimney, making the fire inefficient, while healthy fats burn steadily and help maintain brain function. The key question is: If fats aren’t the enemy, is something else to blame?
Are Carbs the Real Fire Starters?
Your brain runs on glucose—a fast-burning fuel. In a healthy system, glucose burns clean like dry kindling, giving quick bursts of energy without much smoke.
But problems arise when glucose is consistently oversupplied:
- Excess glucose contributes to oxidative stress and insulin resistance, conditions linked to Alzheimer’s disease.
- Some scientists have even labeled AD as “Type 3 Diabetes”, since people with the disease often show impaired glucose metabolism in the brain.
Yet, not all carbs behave the same way. Whole-food sources of carbohydrates (like vegetables, legumes, and whole grains) don’t trigger the same metabolic chaos as refined sugars. This raises an important question: If not all carbs are bad, could there be one type that is particularly harmful?
Is Fructose the Hidden Lighter Fluid of Neuroinflammation?
While most people think of sugar as just glucose, modern diets include large amounts of fructose, a different kind of sugar found in fruit juices, sodas, and processed foods containing high-fructose corn syrup (HFCS).
Unlike glucose, fructose bypasses normal energy regulation and gets rapidly converted into fat and uric acid, both of which are linked to inflammation. New research (Shen et al., 2025) reveals an even more alarming connection:
- Fructose directly activates microglia, the brain’s immune cells, through the GHSR receptor, triggering NF-κB and p38 MAPK pathways—both key drivers of neuroinflammation.
- Fructose metabolism in the brain leads to oxidative stress and lipid accumulation, impairing cognitive function.
- Uric acid, a byproduct of fructose metabolism, worsens inflammation and damages neurons.
In our fireplace analogy, fructose isn’t just dry kindling—it’s lighter fluid. It makes the fire burn out of control, producing toxic smoke (inflammation) that damages brain cells over time.
Could this be why Alzheimer’s rates are rising alongside increased fructose consumption? And if so, is targeting fructose metabolism a viable way to slow the disease?
Mediterranean Diet vs. Ketogenic Diet: Which One Fuels the Brain Better?
Both the Mediterranean diet and the ketogenic diet are often discussed as brain-healthy eating patterns, but they work in very different ways.
- The Mediterranean diet is based on whole grains, vegetables, fruits, fish, nuts, and olive oil, with moderate amounts of protein. It allows healthy carbs, focusing on unprocessed foods while avoiding refined sugars. Research strongly supports it for heart health, brain longevity, and reduced inflammation.
- The ketogenic diet (keto), in contrast, is a low-carb, high-fat diet that drastically reduces carbohydrate intake (often below 50g per day). By doing this, the body shifts from using glucose as its main energy source to producing ketones from fat, which can fuel the brain. Some studies suggest this can help stabilize blood sugar, reduce neuroinflammation, and improve cognitive function in early Alzheimer’s disease.
The key difference? The Mediterranean diet still includes carbs but focuses on high-quality sources, while keto eliminates most carbs altogether. This makes keto more restrictive and difficult to sustain long-term, whereas the Mediterranean diet is more balanced and evidence-backed for overall health and longevity.
What Happens When the Fireplace Malfunctions?
Understanding Alzheimer’s Disease
Alzheimer’s disease is not just about memory loss—it’s a metabolic and inflammatory disorder with several key components:
- Amyloid-Beta Plaques & Tau Tangles = A Clogged Chimney
- Microglial Overreaction = Too Much Smoke
- Mitochondrial Dysfunction = The Fire Burns Out of Control
Could reducing fructose intake be a way to slow this process? And if the brain struggles to use glucose efficiently, does that mean ketogenic diets might help?
What’s the Best Way to Keep the Fire Burning Right?
🔥 Cut Back on Processed Fructose – Avoid HFCS, sodas, and processed sweets.
🔥 Choose Healthy Fats – Olive oil, nuts, and omega-3-rich fish are brain-friendly fuels.
🔥 Use Carbs Wisely – Stick to whole-food carbs while minimizing refined sugar.
Conclusion: Can We Keep the Fire Burning Without Destroying the House?
Neuroinflammation is complex, but the latest research suggests fructose may be one of the most overlooked contributors. While extreme diets like keto may work for some, a balanced, whole-food diet remains the most sustainable choice for long-term brain health.
So, what do you think? Is fructose the hidden culprit behind Alzheimer’s and inflammation? Could reducing it be the missing piece in preventing neurodegeneration? Let’s discuss!
Recent Research on Fat, Glucose, and Fructose in Neuroinflammation and Alzheimer’s Disease
1. Do microglia metabolize fructose in Alzheimer’s disease?
📄 AM Sturno, JE Hassell Jr (2025).
🔗 Read Full Paper
2. Sugar utilization by microglia in Alzheimer’s disease
📄 KM Marino, DC Shippy, TK Ulland (2025).
🔗 Read Full Paper
3. Could Alzheimer’s disease be a maladaptation of an evolutionary survival pathway mediated by intracerebral fructose and uric acid metabolism?
📄 RJ Johnson, DR Tolan, D Bredesen, M Nagel (2023).
🔗 Read Full Paper
4. Western diet induces impairment of liver-brain axis accelerating neuroinflammation and amyloid pathology in Alzheimer’s Disease
📄 A Wiȩckowska-Gacek (2021).
🔗 Read Full Paper