Imagine the brain as a vast landscape of interconnected hiking trails. Some paths are well-trodden, smooth, and easy to navigate—these represent the strong neural connections we use daily. Others are faint, overgrown with weeds, or even blocked, symbolizing the synapses that weaken over time or due to neurodegenerative diseases.
This ability of the brain’s pathways to strengthen, weaken, or reroute is called synaptic plasticity—the brain’s way of adapting and rewiring itself. It plays a crucial role in learning, memory, and recovery from injury. But just like hiking trails, neural connections require maintenance to stay functional. This is where Transcranial Magnetic Stimulation (TMS) comes into play—a high-tech tool that acts as a ‘trail maintenance crew’ for the brain.
How Do We Build and Lose Neural Trails in the Brain?
When we learn a new skill or recall a memory, it’s like walking a new trail. The more frequently we use it, the clearer and more efficient the path becomes—mimicking long-term potentiation (LTP), where synapses strengthen through repeated use. Conversely, trails that remain untouched for long periods become overgrown, just as unused neural connections weaken through long-term depression (LTD).
In neurodegenerative diseases like Alzheimer’s or Parkinson’s, the brain’s ability to maintain and repair these trails deteriorates. Paths that were once well-maintained begin to erode, making it harder to recall memories, control movement, or process information.
Can TMS Act as a ‘Trail Maintenance Crew’ for the Brain?
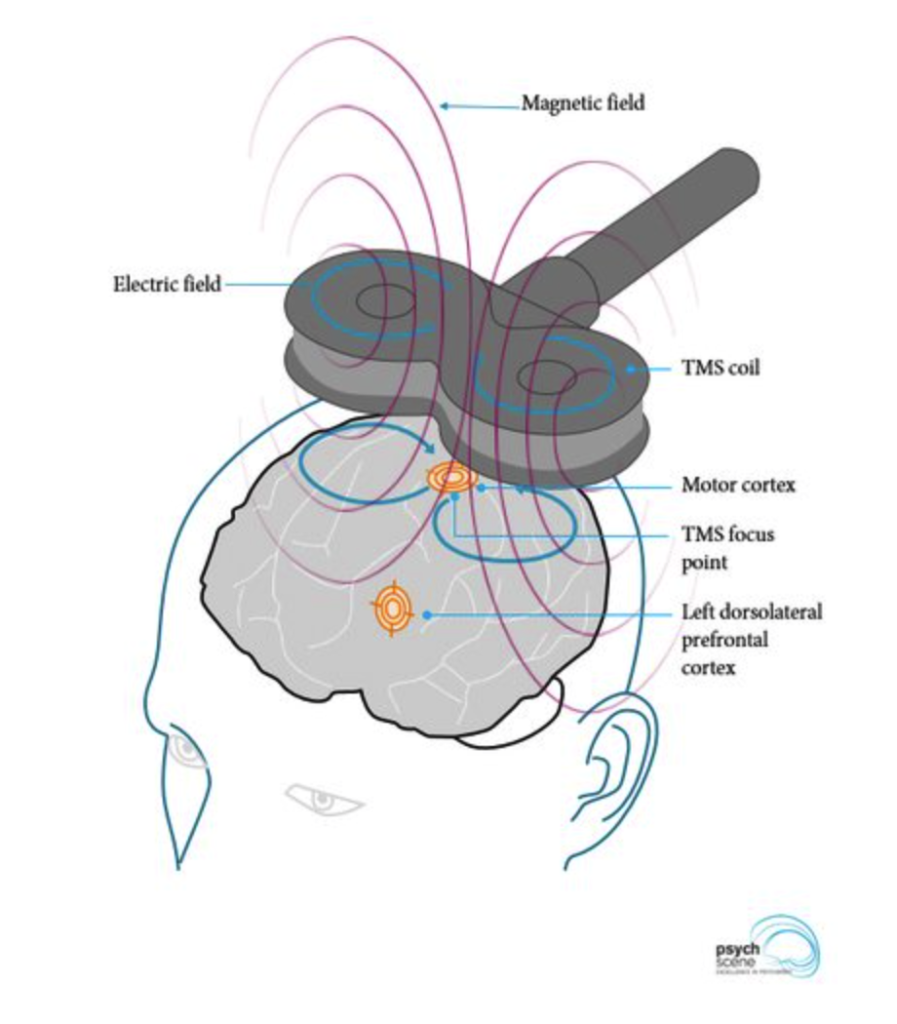
TMS is like sending a specialized crew to clear blocked trails and reinforce frequently used ones. This non-invasive technique uses magnetic pulses to stimulate specific brain areas, influencing synaptic plasticity in different ways:
High-frequency TMS (excitatory stimulation) acts like adding wooden steps and clearing debris from a well-used trail, making it easier to traverse. This strengthens synaptic connections, potentially improving memory, motor function, and cognitive flexibility.
Low-frequency TMS (inhibitory stimulation) slows down overactive pathways, like restricting access to an overused trail to prevent further erosion. This can help balance brain activity, particularly in conditions like depression or movement disorders.
What Role Do Microglia Play in Maintaining Neural Trails?
Recent research has uncovered a new player in this process: microglia, the brain’s resident immune cells. A groundbreaking study titled “Microglia Mediate rTMS-Induced Synaptic Plasticity” reveals that microglia are not just passive responders but active participants in shaping neural circuits through rTMS. These cells act as the brain’s trail keepers, monitoring pathways, removing debris (damaged synapses), and regulating traffic (neuronal activity).
How Does rTMS Affect Microglia and Synaptic Plasticity?
rTMS significantly influences microglial function, particularly in shaping neural plasticity through cytokine release.
Different stimulation protocols and network states modulate microglial response, suggesting a complex interaction between external stimulation and endogenous immune signaling.
What Are the State-Dependent Effects of Microglia on the Brain?
In healthy brain conditions, microglia support synaptic remodeling and neuronal excitability.
In brain injury models, rTMS alters microglial-mediated neuroinflammation, potentially aiding recovery.
How Can TMS Induce Therapeutic Changes in the Brain’s Pathways?
rTMS-induced microglial modulation could be harnessed for therapeutic interventions targeting neuroplasticity.
The findings suggest the need for personalized rTMS protocols that consider microglial activity in different brain regions.
Can TMS and Microglia Modulation Help the Brain Recover from Neurodegeneration?
By integrating these insights, researchers are now exploring how microglial-targeted rTMS protocols could enhance recovery from neurodegenerative diseases. Just as a blocked hiking trail may force hikers to find an alternate route, TMS—by modulating microglia—may encourage the brain to establish new neural pathways, compensating for damaged areas.
💡 For more insight on the latest research of the impact of rTMS in microglia modulation, click here.
Alzheimer’s Disease: Why Do Memory Paths Become Blocked in the Brain?
In Alzheimer’s disease, the brain’s hiking trails begin to erode due to the accumulation of amyloid plaques and tau tangles, which disrupt the connections between neurons. The pathways of memory and learning, once well-maintained and easily traversed, become overgrown with debris, making it difficult to recall important landmarks of our past. Just as a hiker might forget the way to their favorite spot after too many blocked or indistinct trails, Alzheimer’s patients struggle to access stored memories and learn new information.
TMS offers a potential solution by acting as a trail maintenance crew, helping to restore function to these deteriorating paths. High-frequency TMS has been shown to enhance synaptic plasticity in areas like the hippocampus, the brain’s memory hub, potentially improving cognitive function and slowing the progression of cognitive decline. Through targeted stimulation, TMS may clear some of the ‘debris’ caused by plaque buildup, making memory pathways easier to navigate and strengthening neural circuits that are critical for recalling information.
💡 For more insight on the latest research, click here.
Parkinson’s Disease: How Do Damaged Motor Trails Affect Movement?
In Parkinson’s disease, the pathways responsible for smooth and controlled movement are damaged due to the loss of dopamine-producing neurons. These motor trails, which once allowed for fluid, coordinated movement, become blocked and overgrown, leading to tremors, rigidity, and bradykinesia (slowness of movement). As if hiking on a trail that has become littered with rocks and obstacles, patients with Parkinson’s struggle to perform even simple motor tasks.
TMS provides a way to clear some of these obstacles by stimulating areas of the brain responsible for movement. High-frequency TMS to the motor cortex can help reinforce the connections between brain regions involved in motor control, improving movement and reducing tremors. By stimulating the brain to ‘re-map’ motor functions, TMS can help patients regain some of their lost abilities, restoring a smoother path for movement and motor coordination.
💡For more insight on TMS as a potential therapy option for Parkinson´s, click here.
Depression: What Happens When Emotional Trails Become Overgrown?
In depression, certain brain regions, such as the prefrontal cortex, can become underactive, while other pathways become overactive. It’s as if some trails are too worn and trodden, constantly being used and eroded, while others fall into disrepair, leading to a state of imbalance. This imbalance results in mood disturbances, negative thought patterns, and difficulty engaging with the world in a positive way.
TMS can help by ‘rebalancing’ these overactive and underactive pathways. Low-frequency TMS applied to overactive regions can reduce excessive activity, like restricting access to a well-worn trail that is eroding, while high-frequency TMS can stimulate underactive areas, like clearing debris from a blocked path, making it easier for positive thoughts and emotions to flow. By promoting synaptic plasticity and enhancing communication between brain regions, TMS offers a promising tool for restoring a healthier emotional landscape.
💡For more insight on TMS as a treatment option for Depression, click here.
Stroke Recovery: Can the Brain Create New Paths After Injury?
After a stroke, the brain’s pathways are disrupted as blood flow to certain regions is cut off. Like a hiker facing a washed-out trail, patients must rely on alternate routes to bypass the damaged areas. Neuroplasticity allows the brain to form new pathways, but this process takes time and effort, and not all paths are easy to establish.
TMS can accelerate this process by stimulating healthy regions of the brain to take over the functions of the damaged ones. High-frequency TMS can promote the growth of new synapses, reinforcing the formation of alternative pathways. This ‘trail maintenance’ helps the brain rewire itself, improving motor, cognitive, and speech recovery. Personalized TMS protocols that consider individual patterns of brain activity and injury can optimize these efforts, helping the brain create more functional routes for recovery.
💡For more insight on TMS as a potential therapy option for Stroke, click here.
How Can We Personalize Brain Stimulation for Better Results?
Biomarkers for microglial activation could help fine-tune stimulation settings to maximize therapeutic outcomes.
What Role Can TMS Play in Neurorehabilitation?
Microglia-targeted neuromodulation could become a promising avenue for enhancing recovery in conditions like Parkinson’s disease, schizophrenia, and depression.
Can TMS and Medications Work Together to Improve Treatment?
Integrating rTMS with pharmacological interventions targeting microglia (e.g., anti-inflammatory drugs) could optimize treatment strategies for stroke, traumatic brain injury, and neuropsychiatric disorders.
What Does the Future Hold for Brain Health and TMS?
While TMS is not a cure, it represents a promising tool in preserving and even enhancing the brain’s natural plasticity. By understanding the brain as a network of trails—constantly evolving and requiring maintenance—we can appreciate the potential of interventions like TMS and microglial modulation in keeping our cognitive pathways clear and functional.