Imagine your brain as a bustling airport, with air traffic controllers guiding planes, security teams ensuring safety, and staff members keeping everything running smoothly. Each part of the airport represents a different brain function—baggage handling for memory, flight schedules for emotions, runways for movement, and control towers for coordination. The immune system acts as the airport’s security force, preventing threats from disrupting operations. But what happens when security mistakes employees for intruders and starts grounding planes, canceling flights, and shutting down terminals? This is the essence of autoimmune encephalitis (AE), a rare but serious condition where the body’s immune system mistakenly attacks healthy brain cells, leading to inflammation and severe neurological symptoms.
Why Does the Brain’s Own Security System Turn Against Itself?
To make sense of AE, let’s expand our airport analogy. In a well-run airport, security ensures passengers and flights move efficiently. However, in AE, security misidentifies essential personnel as threats. They remove baggage handlers (leading to memory problems), detain pilots (causing movement disorders), and shut down runways (disrupting coordination). With each misstep, the airport plunges into chaos—flights are delayed, connections are missed, and the entire system grinds to a halt, much like how AE disrupts brain function.
What Are Autoantibodies and How Do They Cause Damage?
Autoantibodies are immune system proteins that mistakenly attack the body’s own cells instead of foreign invaders. In AE, these autoantibodies target key brain receptors, such as NMDA receptors (involved in memory and cognition) or LGI1 and CASPR2 (which help regulate brain signaling). This leads to disrupted communication between neurons, causing symptoms like confusion, seizures, and movement disorders. It’s as if the airport’s security team receives a false report and starts detaining essential workers, shutting down operations in the process.
What’s Happening Behind the Scenes? A Deeper Look Into the Pathophysiology
Now, let’s zoom in on a key area of the brain: the dura mater—the outermost protective layer, like the airport’s security perimeter. Recent research shows that the dura mater isn’t just a passive barrier; it actively monitors and manages immune activity, much like an airport’s security team managing passenger flow and potential threats. Factors like gut microbiota imbalances can influence immune responses here, further complicating AE.
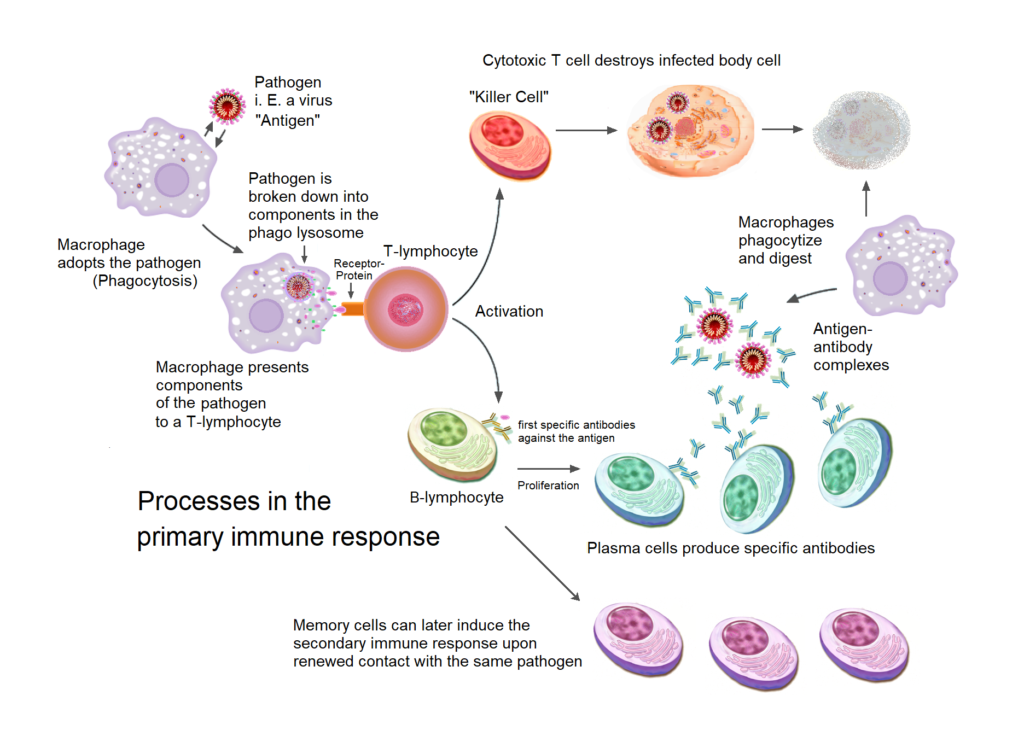
Which Immune Cells Are Involved in the Attack?
T Cells (CD4⁺ and CD8⁺ T Cells): The Overzealous Security Officers
- CD4⁺ T helper cells (Th17 and Th1) act like overzealous security managers, raising alarms (by releasing inflammatory signals like IL-17 and IFN-γ) even when there’s no real threat, leading to unnecessary crackdowns on airport staff (neurons).
- CD8⁺ cytotoxic T cells act as enforcers, aggressively detaining innocent workers (neurons), leading to operational breakdowns in the airport (brain damage).
B Cells and Plasma Cells: The Misinformed Investigators
- B cells are like investigators who get false intelligence and mistakenly identify regular employees as threats.
- They produce autoantibodies (such as anti-NMDA receptor, LGI1, and CASPR2 autoantibodies) that lead to wrongful arrests of key staff members, shutting down airport operations (disrupting neuronal communication).
- The dura mater serves as a hidden operations room where these faulty investigations continue, fueling ongoing disruption.
Macrophages (M1 and M2): The Reactive Crisis Teams
- M1 macrophages act like crisis teams that overreact to false alarms, releasing inflammatory messages (TNF-α, IL-6, IL-1β) that break security barriers (damaging the blood-brain barrier, allowing more trouble into the airport/brain).
- M2 macrophages normally repair damage, but in AE, their instructions get mixed up, making repairs ineffective or even counterproductive.
Dendritic Cells (DCs): The False Alarm Triggers
- These cells act like misinformed airport security scanners, wrongly flagging harmless personnel and alerting T cells to attack them, escalating the crisis unnecessarily.
Meningeal Innate Lymphoid Cells (ILCs): The Protesters
- ILC3 cells are like a group of protesters that amplify the security overreaction by encouraging more unnecessary detentions (by releasing IL-17, fueling inflammation).
Mast Cells: The Chaos Instigators
- Located in the dura mater, mast cells are like staff members who pull fire alarms at the first sign of trouble.
- They release histamine and inflammatory signals that increase crowd panic (vascular permeability), leading to more immune cells storming in and making things worse.
How Does Dura Mater Inflammation Contribute to AE?
The dura mater is like an airport’s outer security perimeter, regulating who enters and exits. When it becomes inflamed, several critical failures occur:
Weakened security barriers (Increased Blood-Brain Barrier Permeability):
The broken security system lets unchecked individuals (autoantibodies and immune cells) flood into the airport (brain), causing widespread chaos.
Excessive alarm signals (Enhanced Cytokine Signaling):
Emergency announcements keep blaring throughout the airport, escalating panic (neuroinflammation) and making it harder for the system to function normally.
Hidden threat bases (B Cell Survival Niches):
Certain areas of the airport (dura mater) continue harboring rogue investigators (B cells), allowing them to keep feeding false information and maintaining the crisis.
Recognizing the Symptoms: A Warning System for the Brain
AE can present with a variety of symptoms, each tied to a specific disruption in brain function:
- Psychiatric changes (sudden mood swings, paranoia, hallucinations): The emotional control tower malfunctions, sending confusing signals to the rest of the airport. Flight schedules (emotional regulation) become erratic, leading to unpredictable behavior.
- Memory loss and cognitive decline (difficulty remembering recent events, trouble concentrating): The baggage handling system (memory storage and retrieval) is compromised, resulting in lost or misplaced information.
- Seizures (uncontrolled electrical activity in the brain): Like power surges shutting down airport systems, seizures occur when neurons fire uncontrollably, disrupting normal communication.
- Speech and movement difficulties (slurred speech, tremors, involuntary movements): When the airport’s communication system and runways are damaged, pilots (motor functions) struggle to navigate, leading to uncoordinated speech and movement.
- Loss of consciousness (in severe cases, leading to coma): If security breaches escalate and the entire airport shuts down, critical functions cease, leading to unconsciousness or coma.
How Does Gut Microbiota Influence AE?
Gut microbiota—the diverse community of microbes in our digestive system—plays a crucial role in regulating immune function. When the microbiota is well-balanced, it helps maintain immune tolerance, preventing unnecessary immune attacks. However, in AE, disruptions in gut microbiota (dysbiosis) can trigger excessive immune activation, leading to increased inflammation in the dura mater. This heightened immune response may contribute to the development and persistence of AE by allowing more autoantibodies and immune cells to enter the brain, exacerbating neurological symptoms.
How Can We Restore Order? A Step-by-Step Breakdown of First-Line Treatments
Corticosteroids: Calming the Overzealous Security Force
- Corticosteroids act as an emergency override, reducing inflammation and stopping unnecessary immune attacks.
Intravenous Immunoglobulin (IVIG): Deploying Specialized Backup Security
- IVIG floods the system with healthy antibodies, neutralizing the autoantibodies causing the crisis.
Plasma Exchange (PLEX): Clearing Out the False Reports
- PLEX physically removes harmful autoantibodies, resetting the immune response and restoring order.
What Are the Best Strategies for Treatment?
- Second-Line Therapies: If first-line treatments fail, stronger measures like rituximab and cyclophosphamide target B cells to prevent further attacks.
- Maintenance Therapy: Long-term immune suppression prevents relapses and ensures stability.
What’s on the Horizon for AE Treatment?
- JAK Inhibitors: These drugs work by blocking Janus kinase (JAK) enzymes, which play a key role in the inflammatory response. By inhibiting these pathways, JAK inhibitors can reduce the immune system’s overactivity and help control AE symptoms.
- CAR-T Cell Therapy: Researchers are exploring engineered immune cells to precisely target and neutralize autoreactive cells.
- Clinical Trials: Ongoing studies aim to refine treatment protocols and introduce new, effective therapies.
Hope for the Future: Can the Airport Return to Normal?
Advancements in AE research are paving the way for more targeted therapies, reducing the risk of long-term damage. With early detection and proper intervention, many individuals can recover and regain their quality of life. By continuing to explore the intricate relationship between the immune system and the brain, researchers aim to restore order in the neural ‘airport’—ensuring every plane can take off and land smoothly once again.




