When you think about your immune system, it’s like your body’s natural defense mechanism. But what happens when the threat—like a brain tumor—has learned how to evade detection? This is where cancer vaccines come in, offering a revolutionary approach to help train the immune system to recognize and fight these dangerous cells.
One of the most exciting advancements in this area comes from mRNA vaccines. To understand how they work, think of cancer vaccines as a “recipe book” that provides your immune system with the precise instructions it needs to identify and fight cancer cells, much like following a recipe to make a delicious meal. In this article, we’ll dive into how cancer vaccines, including mRNA vaccines, can help equip our bodies to fight brain tumors and beyond.
What Are Cancer Vaccines, and How Do They Work?
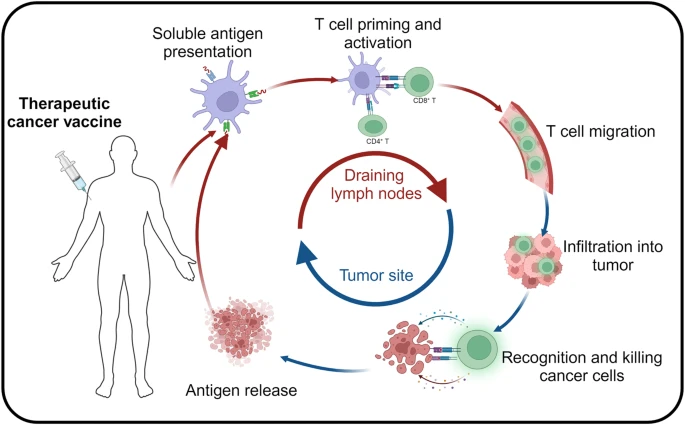
Cancer vaccines are designed to give the immune system a “recipe book,” providing step-by-step instructions needed to recognize and destroy cancer cells. But how does this recipe book work, and how do different vaccines approach this task? Just like a recipe book that’s updated to include new, healthier ingredients, cancer vaccines provide the immune system with the latest instructions on how to identify tumor cells and fight them. Let’s explore the different types of cancer vaccines used in neuro-oncology.
Types of Cancer Vaccines in Neuro-Oncology
Think of cancer vaccines as different cooking techniques that help prepare your immune system to identify specific threats, much like how various recipes teach you to create different types of dishes. Here are the main types of cancer vaccines currently being researched in neuro-oncology, specifically for brain tumors:
Peptide-Based Vaccines – Adding Key Ingredients
Peptide-based vaccines are like adding key ingredients to a dish that enhance its flavor. These vaccines provide small pieces of proteins (called peptides) found on the surface of the tumor. The immune system then learns to recognize these peptide “ingredients” as signals of cancer, helping it target and destroy tumor cells. For instance, the SurVaxM vaccine targets a protein called survivin, which helps tumor cells avoid destruction, teaching the immune system to spot and eliminate glioblastoma cells.
Dendritic Cell Vaccines – Hiring a Master Chef
Dendritic cell vaccines are like hiring a master chef to teach you how to prepare a specific dish. Dendritic cells act as the immune system’s “taste testers,” helping the immune system recognize what’s dangerous and what’s not. In vaccines like DCVax-L, a patient’s own dendritic cells are harvested, loaded with tumor-specific information, and then reinfused to enhance the immune system’s ability to recognize and fight brain tumor cells. This personalized approach has shown promising results in clinical trials for glioblastoma patients.
💡 For a deeper dive into Dendritic Cell Vaccines, click here to read my blog post.
mRNA Vaccines – Real-Time Recipe Updates
Finally, mRNA vaccines work like receiving a real-time recipe update that teaches your immune system how to recognize and fight evolving cancer threats. Instead of delivering proteins directly, these vaccines provide genetic instructions to your cells, teaching them how to produce a specific cancer protein. The immune system then learns to recognize these proteins and attack the tumor cells effectively.
Understanding mRNA Vaccines: A Recipe for Immune Success and a New Hope for Brain Tumor Treatment
Now that we’ve covered the basics of different cancer vaccine types, let’s take a deeper look at mRNA vaccines and explore what makes them so revolutionary for cancer treatment, particularly in the fight against brain tumors.
What Makes mRNA Vaccines Unique for Cancer Treatment?
In recent years, mRNA vaccines have become a household name, primarily due to their groundbreaking role in combating COVID-19. But did you know that the same technology is being explored as a potential game-changer for cancer treatment, including brain tumors? Whether you’re new to mRNA vaccines or you’re curious about their impact on neuro-oncology, this article breaks it down in simple terms while shedding light on the latest research pushing the boundaries of cancer treatment.
What Exactly Is mRNA, and Why Should We Care About It?
To understand the potential of mRNA vaccines, we first need to explore the fundamental role of mRNA in our body.
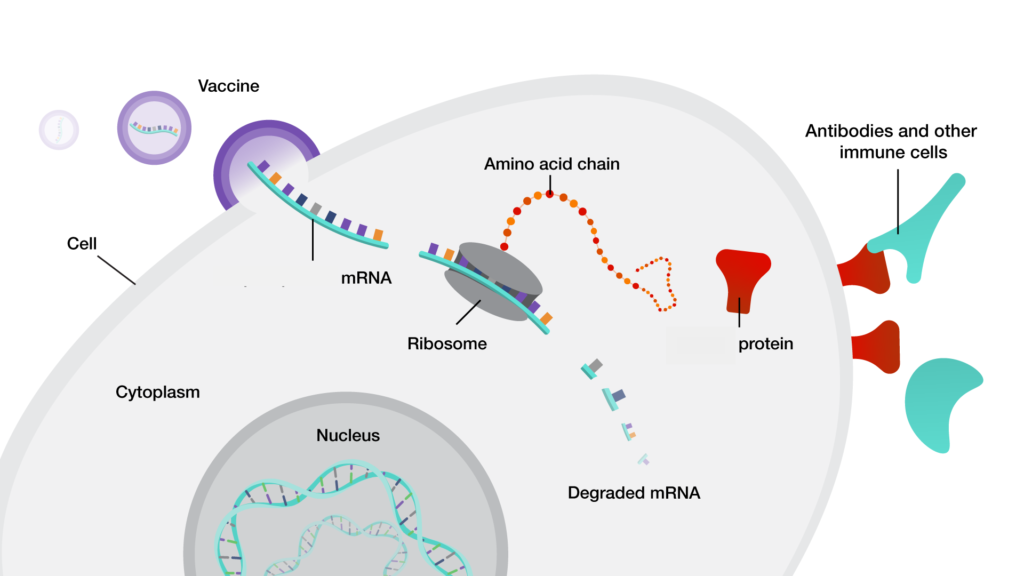
mRNA (messenger RNA) is a vital type of genetic material that serves as a messenger between our DNA and the protein-making machinery inside our cells. Imagine mRNA as a “recipe” or “instruction manual” carrying genetic instructions from our DNA to the ribosomes, which act as the “protein factories” in the cell.
Here’s the key: proteins are responsible for nearly every function in our body—from building muscle to defending us against infections. But our cells can’t just create proteins out of thin air; they need precise instructions. This is where mRNA steps in, translating the genetic code from our DNA into actionable blueprints for protein production.
So, when our DNA needs to create a protein, it first gets transcribed into mRNA. This mRNA then leaves the nucleus and heads to the ribosomes, “the protein factories” of the cell, where it is “translated” into the necessary protein that supports various essential functions.
How Can mRNA Vaccines Teach Our Immune System to Fight?
Now that we’ve covered the basics of mRNA, let’s look at how mRNA vaccines utilize this natural process to train our immune system.
Think of an mRNA vaccine as a “recipe book” for your immune system, teaching it to recognize and fight off specific threats—such as viruses or cancer cells. Instead of injecting the actual virus or tumor cells, the vaccine contains mRNA instructions for producing a harmless part of the invader, like the spike protein of the COVID-19 virus or a specific protein found on the surface of a cancer cell.
Once the mRNA is inside our cells, the ribosomes follow the instructions to produce that harmless protein. In turn, our immune system identifies it as an intruder, prompting it to mount a defense against it. This “training manual” essentially prepares the immune system to recognize and fight the real invader if it shows up later.
Because this process uses the body’s own protein synthesis mechanisms (transcription and translation), there is no need to inject an actual virus or tumor cells. The immune system is simply trained by making a harmless piece of the invader and teaching the body how to fight it.
How Are Researchers Enhancing the Immune System’s Ability to Fight Cancer?
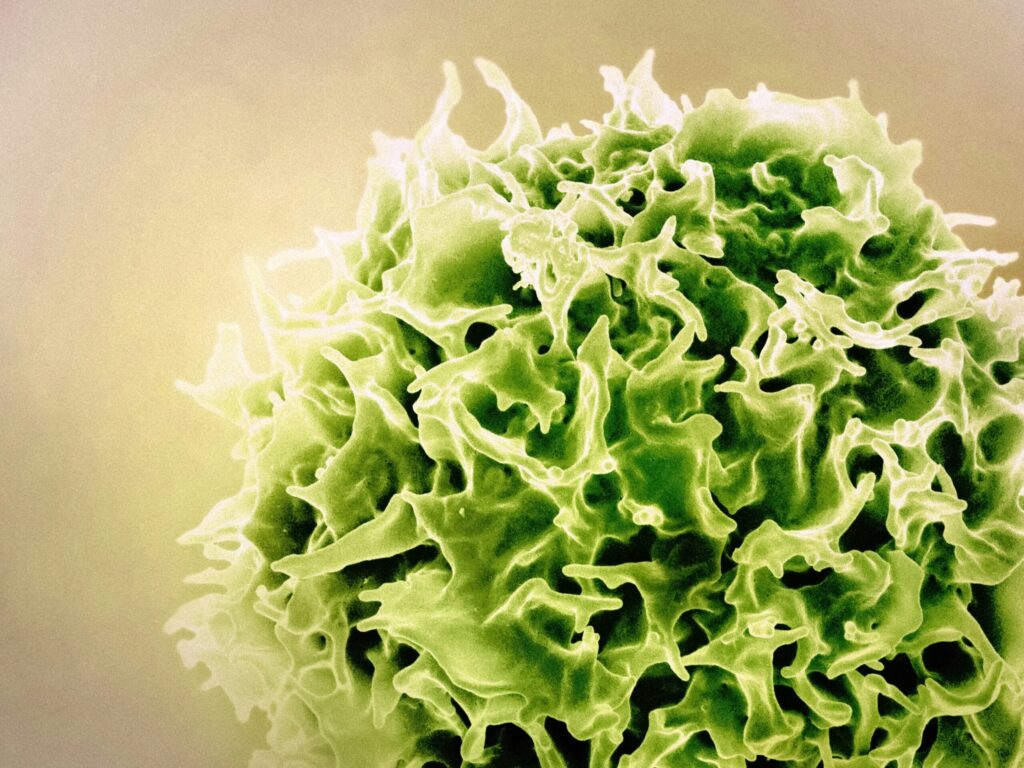
Imagine your immune system as a highly skilled army, but one that sometimes struggles to identify cancer cells—especially those within brain tumors. Tumors often create a “shield,” making it difficult for the immune system to target them. So, how can scientists help the immune system see through this protective barrier?
The answer lies in a new technology known as RNA-Lipid Particle Aggregates (RNA-LPAs). Think of RNA-LPAs as specialized “delivery trucks” that not only transport the mRNA more efficiently but also amplify the immune response to make sure the immune system is fully mobilized.
Unlike traditional mRNA delivery methods, RNA-LPAs are designed to stimulate a stronger immune reaction by activating a key component of the immune system. This can be likened to sending in reinforcements to bolster the army’s fight. In animal studies, including trials with dogs suffering from terminal brain tumors, a single dose of RNA-LPAs improved survival rates and ignited immune activity that made the tumor environment “hot” with immune cells—meaning the tumor could no longer evade detection.
What’s even more exciting is that, in early trials with human patients suffering from glioblastoma (a type of aggressive brain cancer), RNA-LPAs showed significant promise. The immune system quickly responded to the tumor, with signs that it was beginning to mount an effective attack. This was a major breakthrough, hinting that RNA-LPAs could help reset the tumor’s defenses and allow the immune system to see it as a genuine threat.
💡For more insight on this research paper, click here
Are We on the Verge of a Breakthrough in Brain Tumor Treatment?
RNA-LPAs are undoubtedly a major advancement in cancer immunotherapy. By improving the delivery of mRNA instructions and reprogramming the tumor’s environment, this innovative approach could lead to more powerful and targeted treatments for brain tumors.
As research progresses, the potential for mRNA vaccines to fight cancer—particularly brain tumors—becomes more promising. The concept of using our own immune system to recognize and destroy tumor cells is not just an exciting possibility; it’s a rapidly emerging reality.
In the future, mRNA vaccines might not only revolutionize how we fight infectious diseases but also become a vital weapon in the battle against cancer.
📚Got you curious? Here are a few more research papers to dive deeper into:
mRNA vaccines in the context of cancer treatment: from concept to application (06.01.25)
This comprehensive review discusses the evolution of mRNA vaccines in cancer therapy, highlighting their potential in treating various cancers, including those affecting the nervous system.
DDEL-01. ENGINEERING mRNA THERAPIES FOR BRAIN TUMORS (11.11.24)
This study explores the development of lipid nanoparticle (LNP) formulations for delivering mRNA therapeutics to brain cells, aiming to enhance the treatment of brain tumors.
This research presents the initial findings from a first-in-human study evaluating the safety and potential efficacy of the mRNA-based vaccine CVGBM in patients with glioblastoma.
Recent progress in mRNA cancer vaccines (28.01.24)
This review highlights recent advancements in mRNA cancer vaccines, discussing their development, challenges, and potential applications in cancer treatment, including neuro-oncology.
mRNA cancer vaccines from bench to bedside: a new era in cancer immunotherapy (18.12.24)
This article explores the transition of mRNA cancer vaccines from laboratory research to clinical applications, emphasizing their role in cancer immunotherapy.
The transformative potential of mRNA vaccines for glioblastoma (26.09.24)
This review discusses the transformative potential of mRNA vaccines specifically for glioblastoma, a common and aggressive brain tumor, highlighting recent research and future directions.
- Advances in nucleic acid-based cancer vaccines (21.01.25)
This article provides an overview of recent advancements in nucleic acid-based cancer vaccines, including mRNA vaccines, and their potential applications in cancer treatment.